Ever wondered why your abdomen feels different after pregnancy like it’s not quite the same as before? You’re not alone—diastasis recti, or abdominal separation, is a common yet often overlooked condition many people experience during and after pregnancy.
In this article, I’ll dive into what diastasis recti is, why it happens, and the steps you can take to support your recovery. Whether you’re preparing for childbirth or navigating postpartum life, understanding how to care for your core can make all the difference in how you feel and move forward.
What is Diastasis Recti?
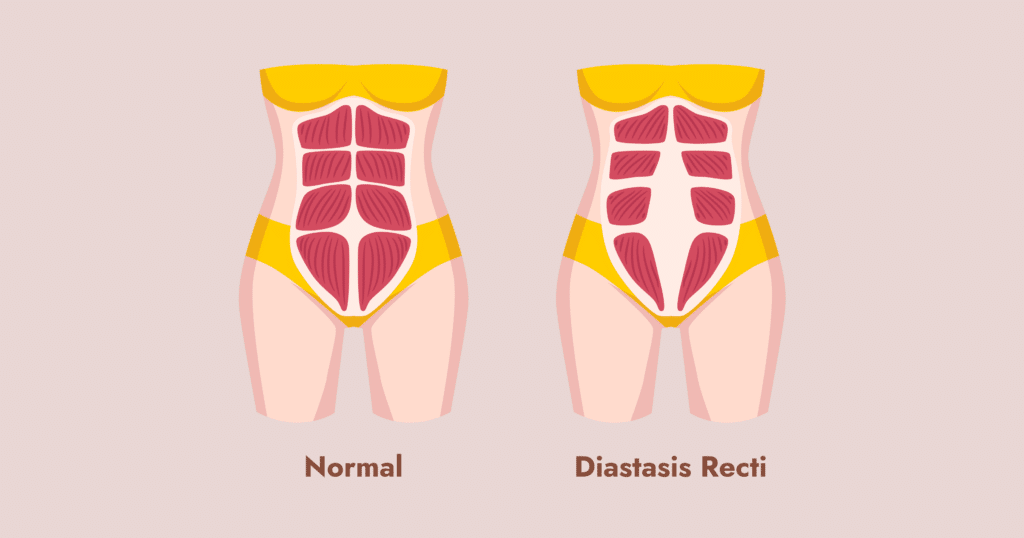
Diastasis recti, or abdominal separation, occurs when the right and left abdominus rectus muscles, which run vertically and connect at the tendinous sheath in the middle (called the linea alba), start to pull apart. This separation happens as your abdomen expands.
The pregnancy hormone relaxin targets collagen (found in tendons, ligaments, skin, connective tissues, scar tissue, and fascia), allowing these fibers to stretch. This helps your hips and other joints become more mobile, assisting in the birthing process as your baby moves into the birth canal.
Some people may become more hypermobile in their tissues than others—this is purely genetic—and may develop diastasis recti more easily during pregnancy.
Other Causes of Diastasis Recti
- Core weakness, particularly in the transverse abdominus muscle, which stabilizes the core and pelvic floor while regulating pressure in the abdomen.
- Pelvic floor weakness or tension.
- Breath-holding or hard bracing of the core during movement or weight lifting (called the Valsalva maneuver), which increases abdominal pressure and can cause a “doming” effect at the center line.
- Poor movement mechanics.
- High-impact activities without proper support, strength, or stability.
- A medical history of hypermobility, such as Ehlers-Danlos syndrome (EDS).
- Genetics.
Some of these factors, like strength, breathing, posture, and exercise choices, can be controlled based on your situation and physiology. However, other factors, like hormones and genetics, cannot.
I always recommend seeing a pelvic physical therapist during each trimester of pregnancy to address changes in your body and to develop a care plan specific to your needs for optimal birth and postpartum outcomes.

Now What About Stretch Marks?
It’s always a good idea to see a dermatologist during pregnancy for a full-body skin check. This is also a great time to ask about evidence-based treatments or modalities for stretch marks if they bother you. Most treatments target fading the marks, though they cannot remove them entirely.
Keeping your abdomen and hips moisturized may help, but in cases where stretch marks are a result of puberty, weight gain/loss, or carrying multiples, sometimes it’s simply genetics or luck.
Should you buy an expensive online “cure” or “prevention” for stretch marks? My advice is to ask your dermatologist and see what treatments are evidence-based before spending your hard-earned dollars on snake oil.
Collagen fibers slide on their filaments, allowing them to stretch. It’s all genetics, babe. In some folks, they slide and bounce back (like a new rubber band). In some, they slide and don’t return to their original position (loose, less elastic, like a stretched-out rubber band); other times, they slide and break at the tension mark (stretch marks or tiger stripes.)
Postpartum Recovery and Diastasis Recti
So, you’ve done due diligence, read Pelvic Prep School for all the facts and prep for pregnancy, birth, and beyond, seen your doctors and a pelvic floor physical therapist, and now you’re postpartum and wondering, how do I go from here?
Here’s what I recommend:
1. Allow your body to heal
Pregnancy and birth represent the greatest physiological changes your body will undergo, even altering your brain size and DNA composition.
I tell my clients that if they had ACL surgery, we’d anticipate it would take a year for the average person to feel fully back to baseline, even with the best care (unless you are a pro athlete or won the genetic lottery, of course).
2. See a mental health therapist who specializes in pregnancy and postpartum
Pregnancy and postpartum may trigger body dysmorphia, eating disorders, and other challenges. For many millennials and GenXers who grew up in 90’s supermodel culture with Seventeen Magazine and Cosmo covers of the “ideal stick thin woman,” a body change can be triggering.
On a personal note, I saw a therapist postpartum because I couldn’t run for the first year (physical issues, sleep deprivation, etc.) after having my daughter. Running was such a big part of my routine, who I am, my community, and my mental and physical health. I really needed help working through losing that part of my identity, even if it was temporary.
Having a child is huge, the transition is huge, and mental health support—whether one-on-one or in a group setting—is a phenomenal resource.
3. See a pelvic physical therapist specializing in postpartum
Diastasis recti (DR) can lead to low back pain, core weakness, postural issues, poor lumbopelvic alignment, pelvic organ prolapse, pelvic pain, bowel dysfunction, and so much more.
When evaluating a client that is postpartum, at Indigo we always look for DR. The old “two-finger test” is not the only indication that DR could be present. It can also look like doming and present in many other ways.
At Indigo, our experts also understand the strong correlation between the pelvic floor and the abdominals. You can do all the exercises you want for DR, but if you aren’t addressing the pelvic floor, you are missing a big part of the picture (and solution).
For postpartum clients, we recommend an internal pelvic floor evaluation with your consent and understanding of the connection.
4. Avoid belly banding (unless cultural)
Wrapping a band around you very tightly without first having a pelvic floor assessment is like squeezing a rubber chicken – it causes pressure to go downward on your pelvic floor, which can lead to pelvic organ prolapse, especially during a time when hormones that make you “stretchy” are more prominent in your body.
The goal of this type of wrapping can be replicated in a different way using different taping methods and breath control.
If you are belly banding for cultural reasons, do the two-finger test and make sure there’s enough wiggle room under the band to prevent above pressure.
These rules don’t apply to a c-section binder postpartum, which should be used as indicated by your provider. Also, high-waisted pants and leggings that provide comfort and support are just fine (no, I’m never going back to low-rise jeans.)
5. Don’t avoid crunches forever
I’ve had clients come to me saying they have been afraid of crunches or certain abdominal exercises, like oblique strengthening, for years because of a fear of diastasis recti and making it worse. This is a little bit of that case of “it depends.”
You want to start by regulating your breath (intra-abdominal pressure), strengthening your deep core muscles, then moving to more global, bigger muscles like the rectus abdominis and the oblique muscles only after being cleared by your pelvic physical therapist. These muscles are crucial to your body; it’s just about strengthening in appropriate ways!
6. Address Diastasis Recti between pregnancies
Another thing I have heard clients say is, “Well, I plan to have more pregnancies, so I will just wait and deal with this once at the end of childbearing.” I don’t recommend this and it has nothing to do with aesthetics and everything to do with how your body will feel during your next pregnancy. We want you to be strong, stable, functional, and feeling good in your next pregnancy!

Final Thoughts
Follow your gut (no pun intended). I’m not here to tell you to “embrace your tiger stripes” or reassure you that your body is a miracle for giving life. You already know that. What I can tell you is that your lifestyle, exercise choices, clothing choices, sexuality, experience in motherhood, and many other aspects are totally unique, and your own lived experience is not exact to anyone else’s.
Your own path, whatever interventions it includes, is yours. Toss that shame in the trash. Educate yourself, reach out to evidence-based resources, and choose what is best for you and your own physical and mental health, your own financial and time resources.
Wherever you are in your journey, Indigo is here to support you.







