Do you go to the bathroom? You have a pelvic floor! Do you engage in intercourse? You have a pelvic floor! Are you a living, breathing human being? You 100% have a pelvic floor! The pelvic floor does not discriminate; people of all genders, all races, and all ages have one!
Your pelvic floor is the unsung hero supporting everyday functions like urination, breathing, and sexual activity.
Despite its integral role, the pelvic floor remains a bit of a mystery to many. So, let’s take a dive into the world of your pelvic floor, where we’ll unravel its complexities, explore its functions, and help you figure out if you might be suffering from a pelvic floor disorder. Plus, we’ll explore how pelvic therapy could benefit you.
So what is the pelvic floor?
The pelvic floor is like a hammock made of muscles and tissues at the bottom of your pelvis, sort of like a sling or a support system. You can think of it as a sling that stretches from the pubic bone to your sit bone.
The pelvic floor has 5 major functions:
- Supporting Organs: Think of the pelvic floor as a supportive hammock for your bladder, bowel, and reproductive organs. It helps keep these organs in place and prevents them from sagging down.
- Controlling Bathroom Habits: The pelvic floor muscles play a key role in controlling when you urinate and poop. They help you hold it in when you need to and relax when it’s time to go.
- Stability and Movement: Beyond its internal functions, the pelvic floor muscles also help with stability and movement. They work together with other muscles in your core and hips to support your body during activities like walking, running, and lifting.
- Blood Flow and Breathing: The pelvic floor muscles also play a role in blood flow and breathing. They help regulate blood circulation in the pelvic area and support the organs involved in breathing, contributing to overall health and well-being.
- Sexual Function: These muscles also contribute to sexual function by helping with arousal and orgasm. To enjoy intercourse and experience orgasms, it’s important that these muscles can contract and relax when they’re supposed to.
Learning more about the crucial functions that your pelvic floor performs is essential because you might one day be affected by pelvic floor dysfunction (PFD).
This is not to scare you but to preventatively equip you with the proper knowledge. This way, you’ll know what to look out for and, even more importantly, what you need to do so you can continue to advocate for the right care.
It’s estimated that 10% of women in their 20s and 30s will be affected by a PFD. This number increases to more than 30% if you’re over 40.
Plus, it doesn’t only affect those assigned female at birth. Fortunately, pelvic floor physical therapy (PT) can treat and prevent a PFD from developing in the first place.
However, awareness about pelvic floor physical therapy is still on the rise, and many people might not be aware that help is available. That’s why it’s so important that we continue to discuss the importance of PT in supporting people throughout the different life stages.
But before we continue, it’s time for a little biology lesson, so sit tight.
Getting to know your pelvic floor
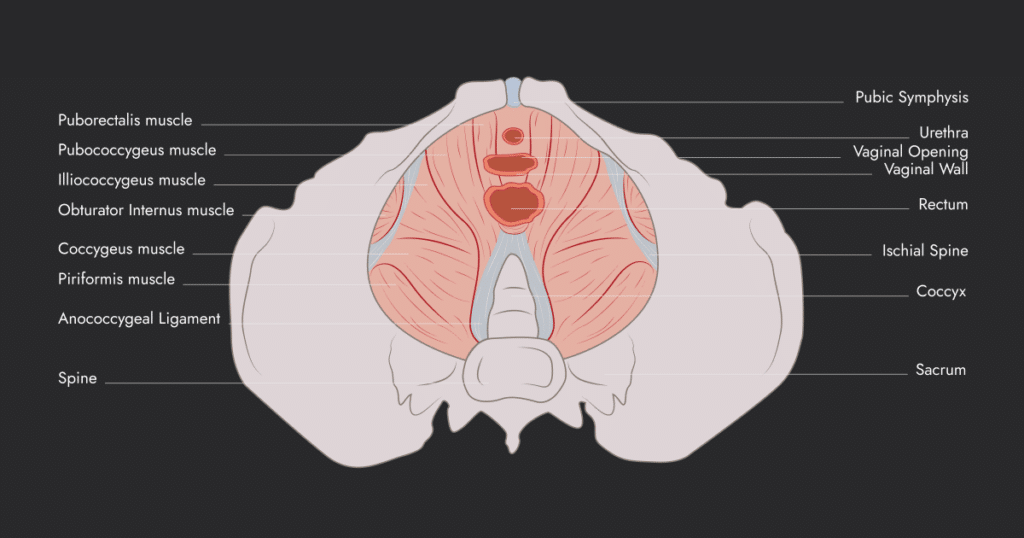
The pelvic floor consists of three layers: the superficial perineal pouch, the urogenital diaphragm, and the pelvic diaphragm.
Layer 1 of the pelvic floor
The superficial perineal pouch, also known as layer 1, is made up of different muscles like the superficial transverse perineal, bulbocavernosus/bulbospongiosus, ischiocavernosus, and the external anal sphincter.
You don’t need to remember all these complicated words, but by understanding the role of each of these muscles, you’ll start to see the fundamental role your pelvic floor plays in keeping your body functioning at its best.
Each of the muscles of your perineal pouch has its own job:
- The superficial transverse perineal muscle helps support and stabilize the perineal body, keeping the pelvic floor strong.
- The bulbocavernosus/bulbospongiosus muscle helps with blood flow during erections and, in those assigned male at birth, it helps with ejaculation and urination.
- The ischiocavernosus muscle also helps with sexual function by delaying the return of blood flow from the clitoris and penis to maintain erections in both males and females.
- The external anal sphincter muscle helps close the anus and lets us control when we go to the bathroom.
Layer 2 of the pelvic floor
The urogenital diaphragm, or layer 2, is made up of two main muscles: the deep transverse perineal and the external urethral sphincter. In people assigned female at birth, there are two additional muscles: the sphincter urethrovaginalis and the compressor urethra.
- The deep transverse perineal muscle supports the perineal body, just like the superficial transverse perineal muscle.
- The external urethral sphincter, sphincter urethrovaginalis, and compressor urethra muscles work together to help with urination and control the flow of urine.
Layer 3 of the pelvic floor
Layer 3 of the pelvic floor, also called the pelvic diaphragm, includes muscles like the levator ani (pubococcygeus, puborectalis, iliococcygeus) and coccygeus.
These muscles work together to support organs in the pelvic area and help with bowel, bladder, and sexual functions.
The coccygeus muscle also supports pelvic organs and aids in bowel movements. Additionally, layer 3 includes muscles in the pelvic walls like the piriformis and obturator internus, which help move your hips in different ways!
Where do pelvic floor disorders occur?
If you are experiencing a pelvic floor disorder, it can occur in any of the layers of the pelvic floor. This means it can originate in the superficial perineal pouch (layer 1), urogenital diaphragm (layer 2), and pelvic diaphragm (layer 3).
These disorders may affect the muscles, ligaments, and connective tissues within these layers, leading to issues such as pelvic organ prolapse, urinary incontinence, fecal incontinence, and pelvic pain.
Your Pelvic Floor’s Allies
Our pelvic floor relies on the support of its counterparts, including our core. Our core is not simply just our abdominal muscles. Instead, it consists of the following:
Abdominal Muscles: Comprising the rectus abdominis, external and internal abdominal obliques, these muscles provide essential support and aid in core stability.
Diaphragm: The primary muscle for breathing, the diaphragm also plays a vital role in core stability and pelvic floor function.
Rib Cage: The rib cage provides structural support and attachment points for several muscles involved in core stability.
Thoracic Spine Musculature: Muscles surrounding the thoracic spine contribute to spinal stability and posture maintenance.
Lumbar Spine Musculature: Muscles around the lumbar spine provide support and stability for the lower back.
Pelvis: The bony structure of the pelvis forms the foundation for pelvic floor support and function.
Deep Hip Rotators: These muscles aid in hip stability and rotation, contributing to overall pelvic support.
Inner Thigh Muscles: Muscles of the inner thigh help maintain pelvic alignment and stability.
Hip Flexors: Essential for hip mobility, the hip flexors also play a role in pelvic tilt and stability.
Gluteal Muscles: The glutes are key for hip extension and pelvic stability.
Hamstrings: These muscles assist in hip and knee movement, supporting pelvic alignment and function.
Understanding the Pelvic Floor Through Postural Support
Understanding the role your pelvic floor plays in your body can sometimes be hard to imagine. To make it easier, Dr. Mary Massery, PT, introduced the “Soda-Pop-Can” Model of Postural Support, which sheds light on how our body responds to internal and external pressures. In this model:
- The top of the can symbolizes the thoracic cavity,
- The middle represents our diaphragm,
- The bottom signifies the abdominal cavity and pelvic floor,
- And the sides of the can denote the abdominal and back muscles.
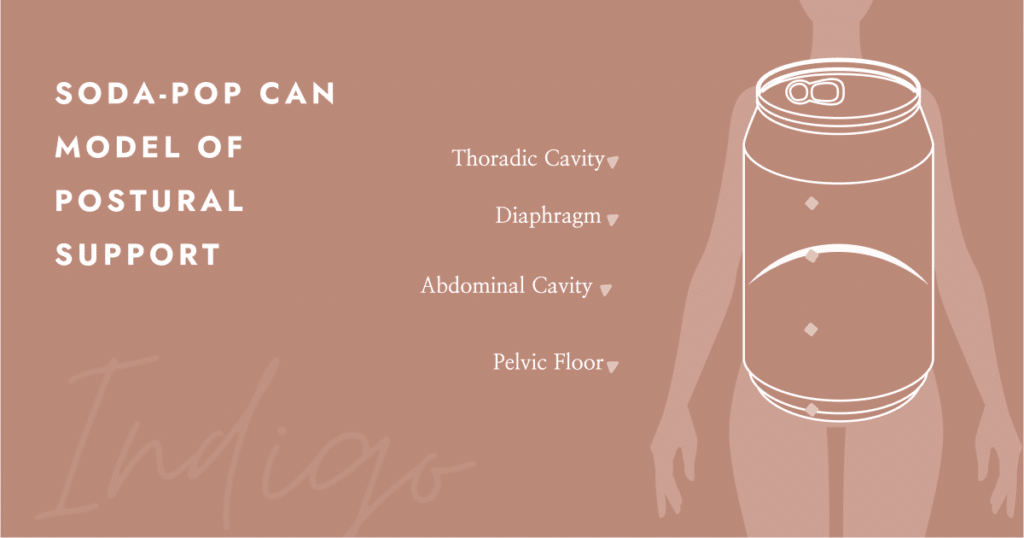
When we breathe in, our diaphragm contracts, pushing down into the abdominal cavity and causing our pelvic floor to lengthen to accommodate the increased pressure. Conversely, upon exhaling, the diaphragm returns to its resting position, leading to a reflexive contraction of the pelvic floor to resume its normal state.
Any dysfunction within our “Soda-Pop-Can,” essentially our trunk, can significantly impact our pelvic floor due to the pressure it experiences. Therefore, maintaining a healthy core, hip muscles, and glutes is crucial.
Remember, our hip muscles, including the piriformis and obturator internus, along with others like the hip extensors, flexors, abductors, and adductors, play a vital role in supporting our pelvis and, consequently, our pelvic floor. Keeping these muscles strong ensures the stability and resilience of our pelvic floor.
Fun fact: The pelvic floor even has connections to the feet and our jaw!
Wondering if you might be suffering from a pelvic floor disorder? Do our quick screening tool.
- As we approach allergy season, are you worried about peeing your pants with sneezing and coughing? Throughout our lives, we have been told that it is normal for females to pee a little when they laugh, sneeze, cough, jump, or exercise of any sort… and that is wrong.
Just because others have told us that it is normal, doesn’t mean that is true and that you have to “live with it”. This is what we call urinary incontinence, when you are unable to hold your pee with changes in pressure and demands placed on your body.
- Do you find yourself straining to have a bowel movement or sitting on the toilet for hours at a time? Or do you experience quite the opposite, where you can no longer hold your bowel movements?
- Do you experience pain or discomfort with intercourse, “squirting”, experience premature ejaculation, or have a difficult time achieving orgasm or an erection?
- Do you have difficulty with inserting a tampon or speculum with pelvic examination or a finger with a prostate exam due to pain?
- Have you ever gone to the doctor for burning with urination and been told your urine culture is negative, but you still have a lingering burning sensation?
- Do you have difficulty starting a urine stream when you are in public settings or any setting? Do you stand up from peeing and dribble a little?
- Do you have a history of endometriosis, PCOS, adenomyosis, or other pelvic floor diagnoses? Have you unfortunately experienced infertility?
- Do you experience heaviness in your pelvic floor, or have been diagnosed by your OBGYN with pelvic organ prolapse?
- Are you currently going through perimenopause or menopause and have symptoms of vaginal dryness, urinary leakage, or pain with intercourse?
- Are you looking to undergo gender reassignment top and/or bottom surgery? Do you experience pain with tucking, binding, or packing?
- Have you had abdominal surgery? Cesarean section? Prostate surgery? Undergone cancer? Hysterectomy? Genital Reconstruction?
- Are you preparing for the birth of your child, just had a child, or unfortunately struggle with infertility?
If you answered yes to any of the above questions, then you experience pelvic floor dysfunction and would greatly benefit from an evaluation with a pelvic floor therapist.
Pelvic Floor Dysfunction (PFD) can occur at various stages of life, but some periods are more prone to its development than others. Understanding when PFD is most prevalent can help individuals take preventive measures or seek timely treatment. Here are some key stages when PFD is commonly observed:
1. Menopause:
The hormonal fluctuations associated with menopause can lead to changes in pelvic floor muscle tone and function. Decreased estrogen levels may contribute to symptoms like urinary urgency, frequency, or stress incontinence in menopausal individuals.
2. Aging:
As individuals age, the pelvic floor muscles naturally weaken and lose elasticity, making them more susceptible to dysfunction. Due to age-related changes, older individuals of all genders may experience urinary incontinence, fecal incontinence, or pelvic organ prolapse.
3. Before and After Pelvic Surgeries:
In the same way that you would do pre-rehab prior to a knee replacement to make the muscles as strong as possible, you would also do this prior to pelvic surgical procedures. These include but are not limited to, prostatectomy, gender-affirming surgeries, hysterectomy, and prolapse.
Surgeries involving the pelvic region can disrupt the integrity of the pelvic floor muscles and surrounding tissues. This may result in PFD symptoms like urinary incontinence, fecal incontinence, pelvic pain or even prolapse post-surgery.
4. Hypermobility:
Patients who experience hypermobility spectrum syndrome or Ehlers Danlos Syndrome are more prone to experience pelvic floor dysfunction.
This may include pelvic organ prolapse, increased tension in pelvic floor muscles, increased joint pain due to more mobility in the joints, impaired proprioception (Proprioception is the body’s ability to sense where it is in space), and potentially chronic pelvic pain.
Patients who experience dysautonomia (a malfunction in the automatic nervous system) may experience slowed digestive tract movement, leading to constipation and bladder retention. This, in turn, leads to increased urinary frequency, urinary urgency and even pelvic pain.
5. Gender Affirming Care:
As individuals prepare for gender-affirming surgeries, it is essential to make sure the pelvic floor muscles have great length and strength prior to and post-surgical procedures.
Patients who experience bottom surgeries need increased education on the tissue healing response and manual therapy to achieve proper dilation of the pelvic floor.
Individuals who are binding, tucking, and packing can also cause or are more likely to experience pelvic floor dysfunction. Pelvic floor therapy is so vital to decrease body dysmorphia that individuals may face.
6. During Pregnancy:
Pregnancy places significant strain on the pelvic floor muscles due to increased weight and hormonal changes.
Plus, if your pelvic floor was either weak or tight before pregnancy, you might find that symptoms are exaggerated by pregnancy. PFD symptoms such as urinary incontinence, pelvic pain, and pelvic organ prolapse are frequently reported during pregnancy.
7. Postpartum Period:
Following childbirth, whether you had a vaginal delivery or even experienced a cesarean delivery, the pelvic floor muscles and abdominal muscles weaken, become overstretched or sustain an injury, leading to various forms of PFD. Issues like urinary or fecal incontinence, pelvic organ prolapse, and perineal pain are common postpartum concerns.
Is Pelvic Floor Physical Therapy Just Kegels?
NO…and honestly, it is quite the opposite for some individuals. Think about the neck muscles right at the top of your shoulders, the upper traps. If you find that your upper traps are already tight and overworked, would you keep performing shoulder raises towards your ears? NO!
Prior to performing kegels, which are pelvic floor contractions, a physical therapist is first going to detect if there is a need for them. Often, kegels can worsen symptoms if relaxation of the musculature is not addressed first!
Like any other muscle group in your body, your pelvic floor muscles can experience imbalances. They can become too tight or not tight enough, leading to various issues.
When the pelvic floor muscles are overly tight, it can result in conditions like pelvic pain, painful intercourse, or difficulty with bowel movements. On the other hand, if these muscles are weak or too relaxed, you might experience urinary or fecal incontinence, pelvic organ prolapse, or decreased sexual sensation.
Achieving the right balance and strength in your pelvic floor muscles is crucial for optimal function and overall well-being.
How will a Pelvic Floor Physical Therapist Assess my Needs?
Pelvic floor physical therapists assess your symptoms from the powerful lens of the pelvic floor, but we keep in mind that the body works as a whole. That means not only evaluating internal and external pelvic floor musculature but taking into account:
- Other joints and musculature (such as knees, feet, ribs, etc.)
- Sitting and standing posture
- Breathing patterns
- Walking and running gait
- Mobility of your skin and fascia
- Alignment of the bones
- Visceral restrictions
- Toileting habits
- Stress
- Exercise
- Diet and water intake
- Overall strength
- Overall flexibility
- Past medical history
We take a look at how all the above areas can play a part in what might be going on at the pelvis. So don’t be surprised when your physical therapist is also assessing outside of the pelvis!
Your pelvic floor physical therapist may choose to utilize a combination of hands-on techniques, neuromuscular re-education, coordination training, mobility, strengthening and stretching to help get you back to being your best possible self.
The therapist may also use a variety of tools, such as myofascial tools, cupping, a TENS unit, kinesiotaping, and even dry needling, to help you achieve your goals.
But at the end of the day, pelvic floor physical therapy entails YOU and your specific needs.